The latest guide on best practices in reproductive medicine, published in September 2023 by the ESHRE (European Society of Human Reproduction and Embryology), recommends against routinely performing Preimplantation Genetic Diagnosis (PGD) or preimplantation genetic testing for aneuploidies (PGT-a). ESHRE analyzes studies published to date and concludes that PGD does not improve live birth rates when compared to conventional IVF cycles with blastocyst transfer, where PGT-a is not performed.
Routine PGD According to Women’s Age
ESHRE’s recommendation generates some conflict as it contradicts the current practice of many reproduction clinics where, increasingly, PGD is routinely offered to women aged 35, 38, or 40 and older, with the hope of reducing the risk of miscarriage and the number of embryo transfers, thereby reducing the time to achieve a successful pregnancy.
Unfortunately, as of today, there are still no well-designed studies that conclusively show that PGD reduces the risk of miscarriage. Only two studies provide results on the time it takes to achieve a successful pregnancy, with no significant differences found between patients who underwent PGD and the control group. More studies analyzing these parameters are needed before drawing conclusions. Let’s review some of the current evidence.
How Many Blastocysts are Needed to Obtain One Chromosomally Normal Embryo?
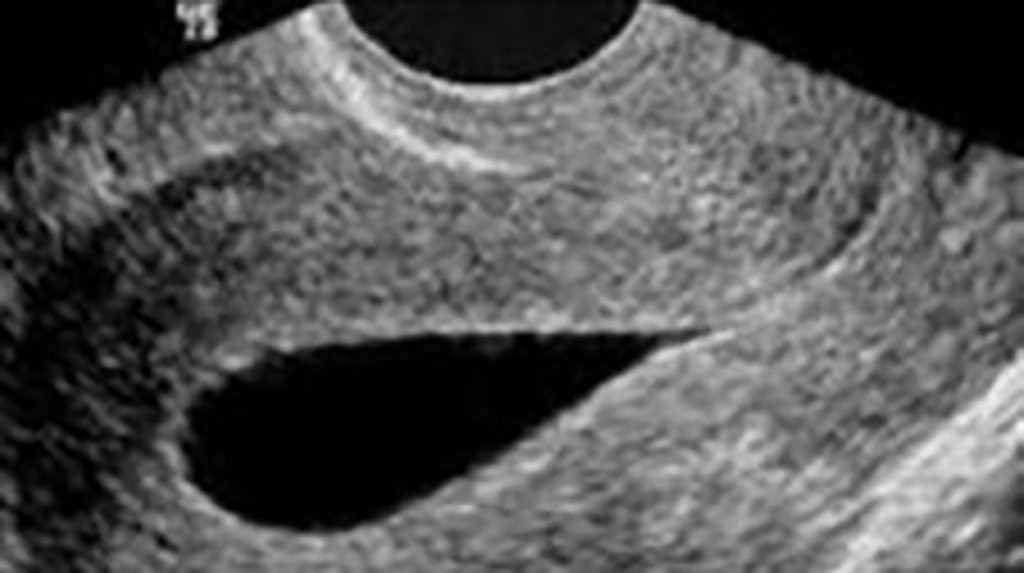
PGD has some associated issues that need consideration. One problem is that some embryos go unanalyzed (reach the blastocyst stage but lack the necessary morphological quality for biopsy) or do not receive a conclusive diagnosis.
As the woman’s age increases, there will be fewer biopsyable embryos in each IVF cycle. Studies, such as the one by Franasiak J.M. et al., covering patients aged 26 to 49 and 3300 cycles, find that 50% of couples have three or fewer blastocysts suitable for biopsy after one IVF cycle. This low number of blastocysts limits the success of the technique.
Additionally, with advancing age, there will be a higher percentage of embryos with genetic abnormalities. The study by Franasiak J.M. provides the number of biopsyable blastocysts needed to obtain one euploid (chromosomally normal) embryo based on the woman’s age:
- Age 35-37: 1.6 blastocysts needed
- Age 38-40: 2.1 blastocysts needed
- Age 41-42: 3.5 blastocysts needed
- Age 43-45: 6.8 blastocysts needed
Does PGD Reduce the Risk of Miscarriage When Routinely Applied?
Unfortunately, transferring euploid embryos does not guarantee pregnancy or reduce the risk of miscarriage in the general population. A 2019 study by Munné et al. included 661 patients aged 25 to 40 and reported a miscarriage rate of 9.9% in the group with the transfer of a euploid embryo (after PGT-a), which was not significantly different from the 9.6% miscarriage rate in the control group (transferring the embryo with the best morphological quality). Results were not significantly different across age groups. The live birth rate was 50% in the PGT-a group and 45.7% in the control group (not a significant difference).
When is IVF with PGD Indicated?
It is considered appropriate to use PGD in couples who have had two or more miscarriages or patients with a history of genetic anomalies.
It is also considered for use in couples with implantation failure, i.e., couples who have not achieved pregnancy after several transfers or a specific number of transferred embryos when the pregnancy prognosis, at their age, with that number of embryos, is greater than 60%.
In reproductive treatments, the quest for solutions to shorten the time to achieve a live-born child is ongoing. This leads to exploring alternatives in patient diagnosis and treatment, which may be considered overdiagnosis and overtreatment. Often, only clinical practice allows us to draw conclusions about the usefulness of each technique. Therefore, staying informed about published clinical studies is crucial. Currently, more information is needed before recommending the routine use of PGD for all patients based on their age. In any case, it is important to analyze each specific case to weigh the pros and cons. At URH García del Real, in line with this premise, we individually assess each couple with the aim of offering the best possible treatment.
If you have more questions about preimplantation genetic diagnosis or any other assisted reproduction topic, URH García del Real offers a free initial consultation. You can request an appointment or call 917401690; we will be happy to assist you.